XLIF®
EXTREME LATERAL INTERBODY FUSION
The thoracolumbar spine is made up of 17 bones, called vertebrae. Twelve vertebrae make up the thoracic (or chest) spine, and five vertebrae make up the lumbar (lower back) spine. Between each vertebra are discs which provide the cushion necessary for spinal rotation and bending. These are called intervertebral discs. Each disc is comprised of two parts, a tough and fibrous outer layer (annulus fibrosis), and a soft, gelatinous center (nucleus pulposus). These two parts work in conjunction to allow the spine to bend, twist, and also provide shock absorption.
What is causing my pain?
There are several primary causes of spine problems. The majority of the symptoms are caused by either instability or by disc, bone, or ligaments pressing onto the nerve roots and/or spinal cord.
What are my treatment options?
Many of the symptoms may be treated without surgery via methods that involve medication, rest, heat, and physical therapy. It is important that you speak to your physician about the best options for you. If your symptoms do not improve with other methods, your physician may suggest spinal surgery.
Surgery is reserved for those who do not gain relief from nonoperative forms of treatment, patients whose symptoms are increasing or worsening, and/or patients that present with a spinal condition which indicates the need for surgery.
What is an eXtreme Lateral Interbody Fusion (XLIF®) procedure?
The eXtreme Lateral Interbody Fusion (XLIF) technique is a minimally disruptive surgical procedure performed through the side of the body. It is designed to treat a range of spinal pathologies. Using patented nerve monitoring technology, the surgeon gains lateral (side) access to the spinal column, avoiding any major nerves in the area between the incision and the column.
The XLIF procedure does not require an anterior (front) or posterior (back) exposure, and thereby does not present the same risks of vascular and/or neural injury as traditional approaches.
Is an XLIF right for me?
If you require spinal surgery, your physician may determine that the XLIF procedure is a good option for you. Some examples of pathologies (conditions) that may be ideal for the XLIF procedure include:
- Degenerated discs and/or facet joints that cause unnatural motion and pain.
- Slippage of one vertebra over another (spondylolisthesis).
- Change in the normal curvature of the spine (degenerative scoliosis).
Conversely, your physician may determine that an XLIF procedure is not a good option for you. It is important to discuss this with your physician in order to determine the best course of treatment for you.
What are the potential benefits of having an XLIF® procedure?
- Smaller incision
- Less blood loss during surgery
- Reduced operative time
- Reduced hospital stay
- Reduced postoperative recovery time
- Significantly increases stability of the spine for long-term healing (fusion)
What can I expect...? Before surgery
Your physician will review your condition and explain all of your treatment options, including medications, physical therapy, and other surgeries such as removal of a diseased disc, fusion, etc. Once you have been admitted to the hospital, you will be taken to a pre-op room and prepared for surgery. This may include instructions about the surgery, cleansing of your surgical site, as well as instructions about the postoperative period.
What happens during surgery?
After you are sedated, positioned on your side, and draped, an x-ray image is taken of your spine to identify the location of the operative disc space.
Step 1. Approach
Your surgeon will make a small incision on the lateral (side) of your body. Dilators will be used to direct the path to the affected disc space while monitoring the local nerves. Once the safest path has been determined, a retractor will be utilized to hold the skin incision open, providing access and visibility to the affected area.
Step 2. Disc Removal
The diseased or damaged disc is removed to reduce pressure from the symptomatic cord or nerve root.
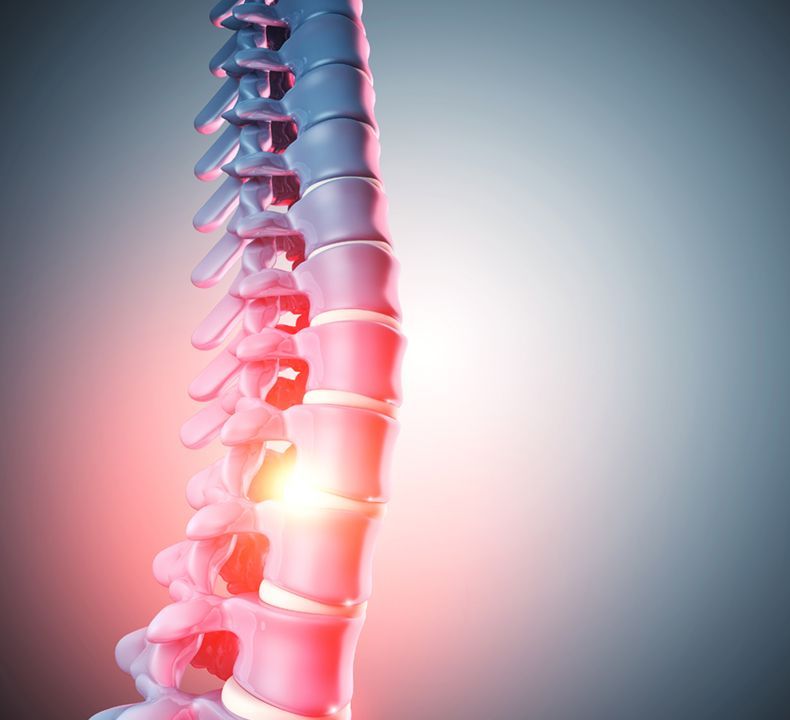
Step 3. Implant
An appropriate implant, chosen by your surgeon, will be placed into the disc space to restore the proper disc height and provide mechanical support while bone grows between the vertebral bodies during the fusion (bone healing) process. That segment of your spine will eventually stabilize once fusion occurs.
Step 4. Fixation
Generally, some method of internal fixation will be used to act as a stabilization device (internal brace) to help hold everything in place while fusion occurs. This could be a combination of screws and plates that are affixed to the adjacent vertebrae. Your surgeon will determine what, if any, kind of fixation is necessary during the procedure.
What can I expect...? After surgery

After surgery you will wake up in the recovery room, where your vital signs will be monitored and your immediate postoperative condition will be carefully observed. Most patients stay in the recovery room between one and three hours after surgery. Once the medical staff feels that you are doing well, you will be returned to your room in the hospital. It is normal for your incision to be sore immediately after surgery.
Most XLIF® patients are discharged from the hospital within 1-2 days after surgery, but your physician will determine the best postoperative course for you. The day after your surgery, your physician may instruct you to use a brace for a period of time to assist with the spinal fusion process. Supervised by trained medical professionals, your physician may ask you to carefully sit, stand, or walk within 24 hours of the surgery. Once you are discharged from the hospital it is important to limit your activities for a period of time (determined by your healthcare provider) to give your body a chance to heal. Your physician will discuss with you any pain medications to take home, as well as a prescribed program of activities. Your physician will provide instructions on wound care, exercises, and limitations to postoperative activity.
Are there risk involved?
Keep in mind that all surgery presents risks and complications that are important to discuss with your surgeon prior to your surgery. Listening to your physician’s guidance, both before and after surgery, will help to ensure the best possible outcome from your procedure.
Potential risks following XLIF® surgery include: problems with anesthesia, infection, nerve damage, problems with the graft or hardware, and ongoing pain. This is not intended to be a complete list of the possible complications. Please contact your physician to discuss all potential risks.